Patients with diabetes are at a higher risk for developing eye conditions as a complication their disease. Over 40 percent of patients diagnosed with diabetes develop some form of eye disease as a result of their disease. Diabetic retinopathy is the most common diabetic eye disease and the primary cause of blindness in the United States.
Diabetes can damage blood vessels in the eye, causing blood or fluid to leak from the retina, the light-sensitive tissue at the back of the eye. It can also cause new blood vessels to grow on the surface of the retina, leading to significant damage to vision and the overall quality of life.
Diabetic eye disease is a combination of various eye conditions that develop as a result of diabetes. These conditions include:

Stages Of Diabetic Retinopathy
There are four distinct stages of diabetic retinopathy. They are:
- Mild nonproliferative retinopathy - microaneurysms develop in the tiny blood vessels of the retina
- Moderate nonproliferative retinopathy - blood vessels to the retina become blocked
- Severe nonproliferative retinopathy - the blood supply to the retina is blocked
- Proliferative retinopathy - New blood vessels, to replace the blocked blood vessels, grow alongside the retina
During any stage of diabetic retinopathy a condition known as macular edema can develop. Macular edema is the buildup of fluid in the macula, the light-sensitive part of the retina that allows us to see objects with great detail. As the macula swells vision becomes blurred. About half of the people with proliferative retinopathy are diagnosed with macular edema.
Symptoms Of Diabetic Retinopathy
Early stages of diabetic retinopathy usually do not show symptoms. Treatment is not always required. Patients need to monitor their blood sugar level to prevent the disease from progressing. If the disease does progress, prompt treatment will be necessary to preserve your vision.
Patients who develop diabetic retinopathy may not notice any changes to their vision at first. In its earliest stages, this condition causes tiny areas of swelling in the small blood vessels of the retina.
Symptoms of diabetic retinopathy may include the following:
- Vision that may be blurry or doubled
- Flashing lights
- Blank spots
- Dark floaters or spots in the vision
- Pain or pressure in either or both eyes
- Problems with peripheral vision
- Severe vision loss or blindness
Who Is Most At Risk For Developing Diabetic Eye Disease?
If you have diabetes, you can develop diabetic retinopathy. These factors increase your risk:
- Longer duration having diabetes
- Poor control of your blood sugar levels
- High cholesterol
- High blood pressure
- Pregnancy
- Tobacco use
- Being African American, Hispanic, or Native American
Can I Prevent Diabetic Retinopathy?
If you have diabetes, it’s not always possible to prevent developing diabetic retinopathy. There are two keys really: controlling your blood sugar and blood pressure and having yearly eye exams with dilation with the team at Southside Eye Care. The goal is to prevent vision loss. The longer you have diabetes, the more likely it is that you will develop diabetic retinopathy.
If you’re diabetic, there are some things you can do to lower your risk of getting diabetic retinopathy:
- Manage your diabetes and blood sugar levels — Take your diabetes medicine regularly as directed. Try to eat a healthy diet and incorporate exercise into your life. You’ll need to test your blood sugar levels several times each day.
- Get an A1C test — Have your doctor call for a glycosylated hemoglobin test, or hemoglobin A1C. This details your average blood sugar level for the two to three months prior to your test. The goal is for A1C to be below 7 percent.
- Keep your blood pressure and cholesterol levels under control — Eating better and exercising regularly helps.
- Don’t smoke
- Pay attention to any vision changes — See an eye doctor if you experience any sudden vision changes or your vision becomes blurry, spotty, or hazy.
What Happens If I Don't Have My Diabetic Retinopathy Treated?
As mentioned above, with the first three stages in the progression of diabetic retinopathy, the only usual treatment is for the patient to manage his or her diabetes. We’ll want to keep tabs on your vision at Southside Eye Care. This is important because most cases of untreated nonproliferative retinopathy will progress to proliferative retinopathy.
That all changes if your retinopathy becomes proliferative. Leaving this stage untreated is putting your overall vision at risk.
Proliferative diabetic retinopathy involves abnormal growth of blood vessels in the retina. This can lead to these complications that can endanger your vision:
- Vitreous hemorrhage — If your new blood vessels bleed into the clear, jelly-like vitreous that fills the center of your eye, this can cause a few dark spots (floaters) or it can block vision if the vitreous cavity fills. This doesn’t necessarily cause permanent vision damage, as the blood often clears. But if it damages the retina, there will be permanent damage.
- Retinal detachment — As your eye develops the abnormal blood vessels, this stimulates the growth of scar tissue. This scar tissue can tug on the retina and pull it away from the back of the eye. This can lead to severe vision loss.
- Glaucoma — If new blood vessels grow in the front of the eye, they can interfere with the normal flow of fluids out of the eye. This causes the pressure inside the eye to build. This is glaucoma and the increased pressure can damage the optic nerve.
- Blindness— Whether due to the diabetic retinopathy or to glaucoma that has developed because of it, the end result can be complete vision loss.
Diagnosis Of Diabetic Retinopathy
After a thorough medical examination of the eyes, some of the following diagnostic tests will be conducted to confirm diagnosis:
- Visual acuity test
- Dilated eye examination
- Tonometry test
- Retinal exam
- Fluorescein angiogram
Are The Treatments For Diabetic Retinopathy Painful?
You won’t feel anything during Dr. Keverline’s treatments. Afterwards, you will have some discomfort, but it’s not acute pain. Most people can get back to their normal activities immediately, although you may have some blurry vision.
Vitrectomies are not painful, but they can be a pain, so to speak. That’s because you may be required to lay face down for a period of time to let your eye heal.
Treatment Of Diabetic Retinopathy
Other than controlling blood pressure, blood cholesterol and the levels of blood sugar, treatment is not needed during the first three stages of diabetic retinopathy. The fourth stage, proliferative retinopathy is treated with a laser surgery procedure known as scatter laser treatment. During the procedure the abnormal blood vessels are ablated causing them to shrink. This procedure works best once the blood vessels begin to bleed.

Severe blood vessel bleeding may need to surgically corrected with a vitrectomy procedure to remove the blood from the eye.
Treatment for macular edema usually includes a laser procedure called focal laser treatment. During this procedure, several hundred small laser burns are placed in the areas of retinal leakage around the macula to prevent leakage from occurring and reduce the amount of fluid in the retina. This helps reduce the risk of vision loss and may improve lost vision in a small number of cases. Focal laser treatment is performed in your doctor's office and can usually be completed in just one session.
What Is Recovery Like After Surgery For Proliferative Retinopathy?
As you would assume, your recovery depends on how Dr. Keverline treated your retinopathy.
With laser treatments, you may have some discomfort and your vision may be blurry for a day or two, but most patients can return to normal activities immediately after these treatments. Some patients experience flashes of light at night or when looking at anything with a white background. These issues will decrease and resolve.
With injections, your visual acuity will also be impacted, but will significantly improve within a week or two. Recovery varies between the different drugs injected.
Vitrectomy requires the most involved recovery, with full recovery taking between 4 to 6 weeks. Some patients may be required to lay face down for a period of time to help their eye heal properly. Typical activities such as driving, reading, and exercise will need to wait for at least a week, maybe more.
Reducing The Risks Of Developing Diabetic Retinopathy
Patients with diabetes need to have an annual comprehensive dilated eye exam. The length of time a patient has diabetes will determine the likelihood of developing diabetic retinopathy. Over 40 percent of patients in the United States, diagnosed with diabetes, have a form of diabetic retinopathy.
The risks of developing diabetic eye disease can be minimized by:
- Monitoring changes in vision
- Keeping A1C levels under 7%
- Monitoring and managing blood pressure levels
- Eating a healthy diet
- Participating in a regular exercise routine
- Monitoring and managing cholesterol levels
Schedule a Diabetic Retinopathy Consultation
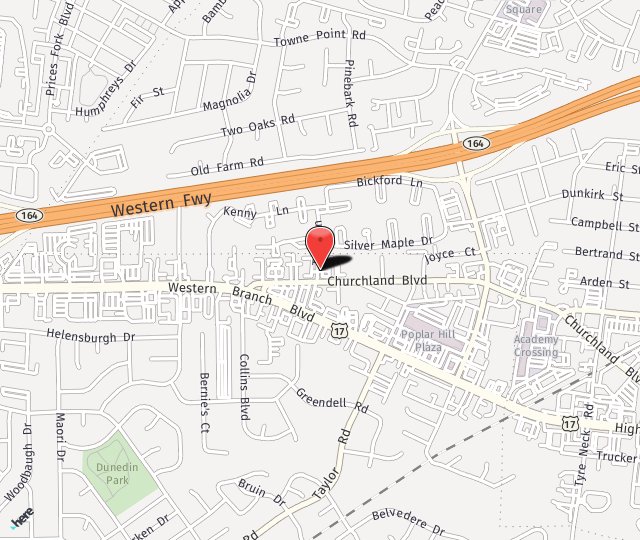
Southside Eye Care proudly serves Chesapeake, Norfolk, Portsmouth, Suffolk and Virginia Beach Virginia as well as the surrounding areas. For more information on Diabetic Eye Disease call us at 757-484-0101 today or fill out our contact form for more information.